The term onychomycosis (fungus of the toenails and fingernails) describes a fungal infection of the nail caused by dermatophytes, non-dermatophytic molds or yeasts. There are four clinically different forms of onychomycosis. Diagnosis is based on examination with CON, microscopy and histology. In most cases, treatment includes systemic and local therapy, sometimes surgical excision.
Factors contributing to nail fungus
- Increased sweating (hyperhidrosis).
- Vascular insufficiency. Violation of the structure and tone of the veins, especially the veins of the lower extremities (typical of onychomycosis of the toenails).
- Age. The frequency of the disease in humans increases with age. In 15-20% of the population, the pathology occurs between the ages of 40-60.
- Diseases of the internal organs. Disturbance of the nervous, hormonal (onychomycosis occurs most often in diabetics) or immune systems (immunosuppression, especially HIV infection).
- A large nail mass, consisting of a thick nail plate and the contents underneath, can cause discomfort when wearing shoes.
- Traumatization. Constant trauma to the nail or injury and lack of proper treatment.
Prevalence of the disease
Onychomycosis– the most common nail disease, responsible for 50% of all cases of onychodystrophy (destruction of the nail plate). Up to 14% of the population is affected, with both the prevalence of the disease in older people and the overall incidence increasing. The incidence of onychomycosis in children and adolescents is also increasing; Onychomycosis accounts for 20% of dermatophyte infections in children.
The increase in the prevalence of the disease may be associated with the wearing of tight shoes, an increase in the number of people receiving immunosuppressive therapy, and the increasing use of public locker rooms.
Nail diseases usually begin with tinea pedis before spreading to the nail bed, where elimination is difficult. This area serves as a reservoir for local relapses or the spread of infection to other areas. Up to 40% of patients with onychomycosis of the toes have combined skin infections, most commonly tinea pedis (approximately 30%).
The causative agent of onychomycosis
In most cases, onychomycosis is caused by dermatophytes, with T. rubrum and T. interdigitale being the causative agents of the infection in 90% of all cases. T. tonsurans and E. floccosum have also been documented as etiological pathogens.
Yeasts and non-dermatophyte molds such as Acremonium, Aspergillus, Fusarium, Scopulariopsis brevicaulis and Scytalidium are the cause of onychomycosis of the toes in approximately 10% of cases. It is interesting that Candida species are the causative agents in 30% of cases of onychomycosis of the fingers, while non-dermatophytic molds are not present in the affected fingernails.
Pathogenesis
Dermatophytes have a wide range of enzymes that act as virulence factors and ensure that the pathogen adheres to the nails. The first stage of infection is adhesion to keratin. The further breakdown of keratin and the cascade-like release of mediators leads to an inflammatory reaction.

The stages of pathogenesis of a fungal infection are as follows.
adhesion
Fungi overcome several host defense lines before hyphae begin to survive in keratinized tissues. The first is the successful adhesion of arthroconidia to the surface of keratinized tissues. The host's early nonspecific defenses include fatty acids in sebum and competitive bacterial colonization.
Several recent studies have investigated the molecular mechanisms involved in the adhesion of arthroconidia to keratinized surfaces. Dermatophytes have been shown to selectively utilize their proteolytic reserves during adhesion and invasion. Some time after adhesion, the spores germinate and move on to the next stage - invasion.
invasion
Traumatization and maceration are a favorable environment for fungal invasion. The invasion of the germinating elements of the fungus ends with the release of various proteases and lipases, generally various products that serve as nutrients to the fungi.
Owner's reaction
Fungi face several protective barriers in the host, such as: B. inflammatory mediators, fatty acids and cellular immunity. The first and most important barrier are keratinocytes, which are encountered by invading fungal elements. The role of keratinocytes: proliferation (to enhance desquamation of horny scales), secretion of antimicrobial peptides, anti-inflammatory cytokines. As the fungus penetrates deeper, more and more new non-specific protective mechanisms are activated.
The severity of the host's inflammatory response depends on the immune status as well as the natural habitat of the dermatophytes involved in the invasion. The next level of defense is a delayed-type hypersensitivity reaction caused by cell-mediated immunity.
The inflammatory response associated with this hypersensitivity is associated with clinical destruction, while a defect in cell-mediated immunity can lead to chronic and recurrent fungal infections.
Although epidemiological observations point to a genetic predisposition to fungal infection, there are no molecular biology-based studies.
Clinical picture and symptoms of damage to the toenails and fingernails
There are four characteristic clinical forms of infection. These forms can occur in isolation or include several clinical forms.
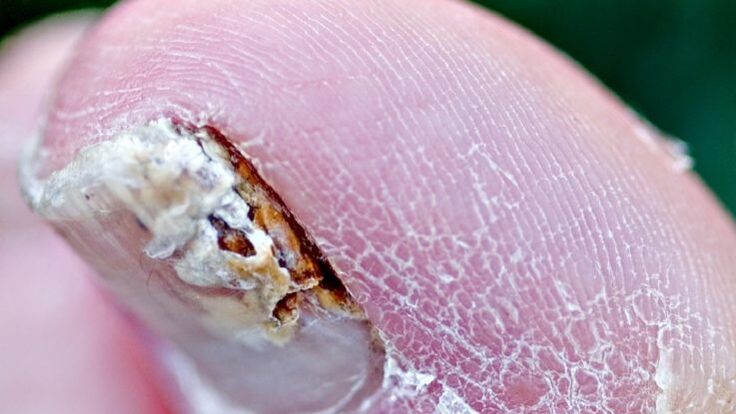
Distal-lateral subungual onychomycosis
It is the most common form of onychomycosis and can be caused by all of the pathogens listed above. It begins with invasion of pathogens into the stratum corneum of the hyponychium and distal nail bed, resulting in whitish or brownish-yellow opacity of the distal end of the nail. The infection then spreads proximally across the nail bed up to the ventral side of the nail plate.

Hyperproliferation or impaired differentiation in the nail bed as a result of a response to infection leads to subungual hyperkeratosis, while progressive invasion of the nail plate leads to increased nail dystrophy.
Proximal subungual onychomycosis
It occurs as a result of infection of the proximal nail fold, mainly by the organisms T. rubrum and T. megninii. Clinic: Clouding of the proximal part of the nail with a white or beige tint. This opacity gradually increases and affects the entire nail, eventually leading to leukonychia, proximal onycholysis, and/or destruction of the entire nail.
Patients with proximal subungual onychomycosis should be examined for HIV infection, as this form is considered a marker of this disease.
White superficial onychomycosis
It arises from direct invasion of the dorsal nail plate and appears as white or dull yellow, well-defined patches on the surface of the toenail. The pathogens are usually T. interdigitale and T. mentargophytes, although non-dermatophyte molds such as Aspergillus, Fusarium and Scopulariopsis are also known to cause this form. Candida species can invade the hyponychium of the epithelium and ultimately infect the nail throughout the entire thickness of the nail plate.
Candida onychomycosis
Damage to the nail plate caused by Candida albicans is only seen in chronic mucocutaneous candidiasis (a rare disease). Usually all fingernails are affected. The nail plate thickens and takes on various yellow-brown shades.
Diagnosis of onychomycosis
Although onychomycosis accounts for 50% of cases of nail dystrophy, it is advisable to obtain laboratory confirmation of the diagnosis before taking toxic systemic antifungals.
Examination of subungual masses with KOH, cultural analysis of nail plate material and subungual masses on Sabouraud dextrose agar (with and without antimicrobial additives), and staining of nail sections using the PAS method are the most informative methods.
Study with CON
It is a standard test for suspected onychomycosis. However, even with a high index of clinical suspicion, it often leads to a negative result, and cultural analysis of the nail material in which hyphae were found during the study with CON is often negative.
The most reliable way to minimize false negatives due to sampling errors is to increase the sample size and repeat the sampling.
Cultural analysis
This laboratory test determines the type of fungus and determines the presence of dermatophytes (organisms that respond to antifungal drugs).

To distinguish pathogens from contaminants, the following recommendations are offered:
- if the dermatophyte is isolated in culture, it is considered a pathogen;
- Nondermatophytic molds or yeast organisms isolated in culture are only relevant if hyphae, spores or yeast cells are observed under the microscope and, without isolation, recurrent active growth of the nondermatophytic mold pathogen is observed.
Culture analysis, PAS – the method of coloring nail clippings is the most sensitive and does not require waiting several weeks for results.
Pathohistological examination
During pathohistological examination, the hyphae lie between the layers of the nail plate parallel to the surface. Spongiosis and focal parakeratosis as well as an inflammatory reaction can be observed in the epidermis.
In superficial white onychomycosis, the microorganisms are located superficially on the back of the nail and display a pattern of their unique "perforating organs" and modified hyphal elements called "bitten leaves. "Invasion of pseudohyphae is observed in Candida onychomycosis. The histological examination of onychomycosis is carried out using special dyes.
Differential diagnosis of onychomycosis
| Most likely | Sometimes probably | Rarely found |
|---|---|---|
|
|
Melanoma |
Treatment methods for nail fungus
Treatment of nail fungus depends on the severity of the nail lesion, the presence of associated tinea pedis, and the effectiveness and possible side effects of the treatment regimen. If nail involvement is minimal, localized therapy is a rational decision. In combination with dermatophytosis of the feet, especially against the background of diabetes mellitus, therapy is absolutely necessary.
Topical antifungals
Local therapy is recommended for patients with distal nail involvement or contraindications to systemic therapy. However, we must remember that local antifungal therapy alone is not effective enough.
Increasingly popular is a varnish from the oxypyridone group, which, when used daily for 49 weeks, achieves mycological cure in about 40% of patients and nail cleaning (clinical cure) in 5% of mild or moderate onychomycosis caused by dermatophytes.
Despite its significantly lower effectiveness compared to systemic antifungal agents, local use of the drug avoids the risk of drug interactions.
Another specially developed medication in the form of nail polish is used twice a week. It is a representative of a new class of antifungals, morpholine derivatives, active against yeasts, dermatophytes and molds that cause onychomycosis.
This product may have a higher mycological cure rate compared to the previous varnish; However, controlled studies are required to determine a statistically significant difference.
Antifungal drugs for oral administration
For onychomycosis in the matrix area or when a shorter duration of treatment or a higher chance of cure and recovery is desired, a systemic antifungal is required. When selecting an antifungal agent, the etiology of the pathogen, possible side effects, and the risk of drug interactions in each individual patient should first be considered.
A drug from the group of allylamines, which has a fungistatic and fungicidal effect against dermatophytes, Aspergillus, is less effective against scopulariopsis. The product is not recommended for Candida onychomycosis because of its variable effectiveness against Candida species.
For most toenail injections, a standard dose of 6 weeks is effective, while toenail injections require a minimum dose of 12 weeks. Most side effects are related to digestive system problems, including diarrhea, nausea, taste changes, and increased liver enzymes.
Data suggest that three months of continuous dosing is currently the most effective systemic therapy for toenail onychomycosis. The clinical cure rate in various studies is around 50%, with treatment rates being higher in patients over 65 years of age.
A drug from the azole group that has a fungistatic effect against dermatophytes and non-dermatophyte mold and yeast organisms. Safe and effective therapies include daily pulse dosing for one week per month or continuous daily dosing, both requiring two months or two courses of therapy for fingernails and at least three months or three pulse therapies for lesions on toenails.
In children, the drug is dosed individually depending on weight. Although the drug has a broader spectrum of action than its predecessor, studies have shown a significantly lower cure rate and a higher relapse rate.
Elevated liver enzymes occur in less than 0. 5% of patients during therapy and return to normal within 12 weeks after stopping treatment.
A drug that has fungistatic activity against dermatophytes, some non-dermatophytic molds and Candida species. This medication is usually taken once a week for 3 to 12 months.
There are no clear criteria for laboratory monitoring of patients receiving the above drugs. It is advisable to have a complete blood count and liver function tests carried out before treatment and 6 weeks after the start of treatment.
A drug from the Grisan group is no longer considered a standard therapy for onychomycosis due to the long duration of treatment, possible side effects, drug interactions and relatively low cure rates.
Combination therapies may result in higher clearance rates than systemic or topical therapy alone. Taking an allylamine drug in combination with the use of a morpholine varnish results in clinical cure and a negative mycological test result in about 60% of patients, compared to 45% of patients receiving only a systemic allylamine antifungal drug. However, another study showed no additional benefit when combining a systemic allylamine agent with a solution of an oxypyridone drug.
Other drugs
The fungicidal activity of thymol, camphor, menthol and Eucalyptus citriodora oil demonstrated in vitro indicates the potential for additional therapeutic strategies in the treatment of onychomycosis. An alcoholic thymol solution can be applied in the form of drops to the nail plate and for hyponychia. The use of local preparations with thymol for the nails leads to healing in individual cases.
surgery
Final treatment options for treatment-resistant cases include surgical removal of the nail with urea. To remove further crumbling masses from the affected nail, special pliers are used.
Many doctors believe that the main and first method of treating nail fungus is mechanical removal of the nail. Surgical removal of the affected nail is most often recommended, less often removal with keratolytic patches.
Traditional methods in the fight against nail fungus
Despite the large number of different folk recipes for nail fungus removal, dermatologists do not recommend choosing this treatment option and starting with a "home diagnosis". It is wiser to start therapy with local drugs that have been clinically tested and proven to be effective.
Course and prognosis
Poor prognostic signs include pain arising from thickening of the nail plate, the addition of a secondary bacterial infection and diabetes mellitus. The most beneficial way to reduce the likelihood of relapse is to combine treatment methods. Therapy for onychomycosis is a long journey that does not always lead to complete recovery. However, do not forget that the effect of systemic therapy is up to 80%.
prevention
Prevention includesa series of events, which allows you to significantly reduce the percentage of onychomycosis infection and reduce the likelihood of a relapse.
- Disinfection of personal and public items.
- Systematic disinfection of shoes.
- Treatment of feet, hands, wrinkles (under favorable conditions - preferred localization) with local antifungal agents as recommended by a dermatologist.
- If the diagnosis of onychomycosis is confirmed, a visit to the doctor for monitoring is necessary every 6 weeks and after completion of systemic therapy.
- If possible, you should disinfect the nail plates at every visit to the doctor.
Diploma
Onychomycosis (fungus of fingernails and toenails) is an infection caused by various fungi. This disease affects the nail plate of the fingers or toes. When diagnosing, examine the entire skin and nails, and also rule out other diseases that mimic onychomycosis. If there are doubts about the diagnosis, it must be confirmed either by culture (preferably) or by histological examination of the nail sections with subsequent staining.
Therapy includes surgical removal and local and general medications. Treatment of onychomycosis is a lengthy process that can take several years. Therefore, you should not expect recovery "from a pill". If you suspect nail fungus, contact a specialist to confirm the diagnosis and prescribe an individual treatment plan.

























